5 Risk factors leading to Bone stress injuries in runners.
Doug James, Physiotherapist, Podiatrist, Marathoner.
A bone stress injury (BSI) is a painful and debilitating problem that affects runners and athletes. It usually occurs as a result of surges in training loads which often coincides with preparing for a competition or a race. Additionally, we’re finding athletes who had to take time off due to Covid-19 quarantine are at greater risk due to a marked reduction in loading during their isolation, and then an overcompensation when returning to running. Depending on the severity of the BSI, the injury may be season ending, or even career ending. The following article will discuss how BSIs develop and the risk factors associated with them.
How they develop
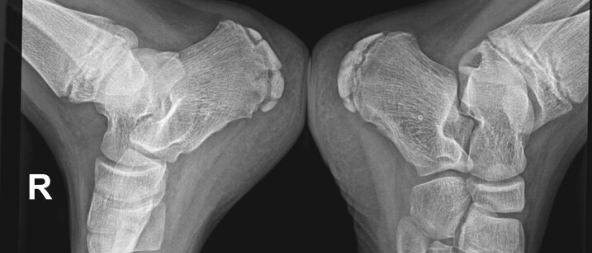
Bone stress injuries occur when the capacity of a bone is unable to deal with the amount of stress it is subjected to [5]. In runners, stress is most commonly generated from running training loads, but any and all physical activity can contribute. If the amount of stress and load is not adequately managed, this can lead to painful fractures developing within the bone. With impact exercises such as running, the bones in our feet, legs, hips and spine undergo stress from compression (jarring from impact when landing), and tension (from muscles absorbing impact, stabilising the body, and creating propulsion). When a healthy bone undergoes sufficient stress that is still within a tolerable level, a process is triggered within the bone to make it stronger. This process involves the removal of part of the bone’s support structure that is then replaced with remodelled and stronger bone.
Symptoms to watch for
In early-stage BSI, symptoms are usually mild – perhaps felt as an ache or light bruising sensation, and might only be felt at the start of physical activity, and/or after the athlete has cooled down. It is thought that at this stage of the injury there is usually only mild damage and a small amount of swelling around the exterior lining of the bone may be evident on MRI. At this stage, the bone’s capacity for loading and stress may be slightly reduced, so caution is needed with any higher risk activities (high-intensity sessions e.g. hills or intervals, or very long runs). If the training load (or other physical activity) continues to stress the bone in its weakened state, swelling within the marrow of the bone begins to develop. At this stage, the injury becomes more uncomfortable during running, but symptoms may still ‘warm up’ as the session continues.
If stress to the bone isn’t reduced sufficiently, the cortical or hard part of the bone begins to degrade and fractures can form within it. By this stage, the injury would be very uncomfortable to run on and is often accompanied by an aching sensation even at rest.
Common BSI sites
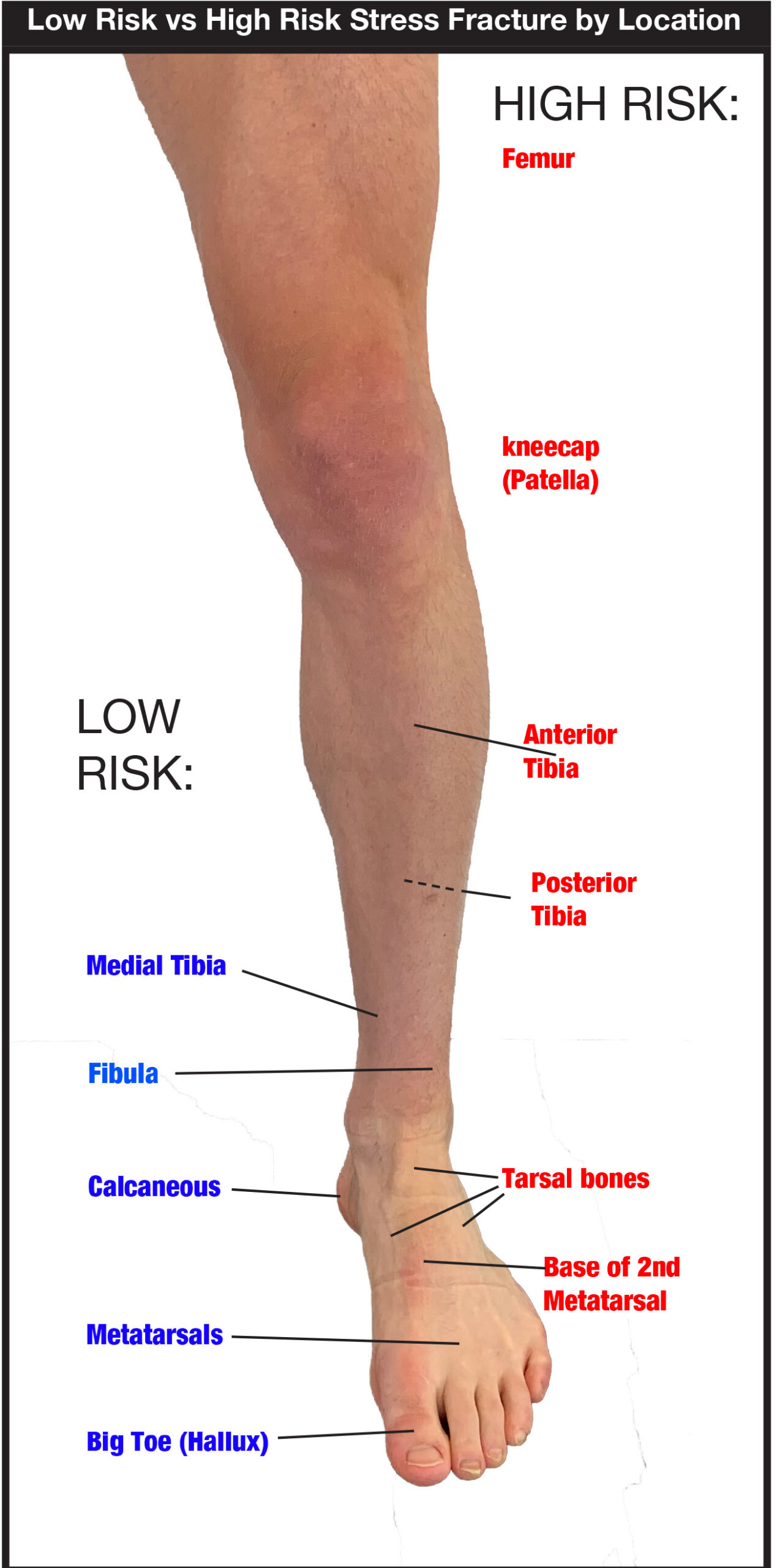
80-95% of all stress fractures occur in the lower limbs[1]. The majority of these lower limb BSI are found in the tibia (shin bone) 33[2]-55%[3], metatarsals (long toe bones in the forefoot) 20%[2], and the remainder in the hindfoot and femur (thigh bone).
Who is at risk
Bone Stress Injuries can account for 50% of injuries sustained by runners and military recruits [3]. Female runners are twice as likely as their male counterparts to develop a bone stress injury [3]. Aside from being female, there are a number of factors that have been identified as risks for developing a bone stress injury.
Risk factor: Training load
By their nature, a BSI requires stress to develop [3]. A rapid increase in training load, particularly in poorly conditioned athletes or those new to running will likely bring about sufficient stress to develop a bone injury. A long history of physical activity is protective [6] as this tends to improve bone density over time. Total training volume needs to be monitored over the course of weeks and months to ensure adequate recovery occurs in order for bones to strengthen. For runners that have taken more than 2 weeks off training due to illness and/or quarantine, a gradual return to pre-break levels is advised. Those that are new to running need to be careful if mirroring the training of more experienced runners.
Risk factor: Running technique
Running technique can play a part in the development and likely location of a BSI. Distance runners who land on their heels are more likely to develop a BSI in the tibia. In contrast, sprinters, and runners who land on their forefoot are more likely to develop a metatarsal (toe bones) BSI.
Runners that produce high ground reaction force (impact)[2,3,4] and had increased rearfoot eversion [4] (rolling in) were more likely to suffer tibial stress fractures. Gait retraining can be beneficial in cases of recurrent BSI but needs to be done carefully due to the risk of injury developing from an unaccustomed running style [6].
Risk factor: Footwear
Shoes can play a role in the development of a BSI. It was found that running in old or worn-out shoes increases the risk of BSI[8]. General footwear industry advice is to replace shoes within 600km of running, but keep in mind that shoes will also degrade over time irrespective of use.
A recent study has proposed that running in maximalist (thickly cushioned shoes such as HokaTM) may reduce the risk of tibial stress fractures in female (but not male) runners. By comparison, minimalist (thinly cushioned) shoes were linked to metatarsal stress fractures(10). The use of foot orthotics was found to help reduce the risk of developing BSI in military recruits[9].
Risk factor: Low energy availability
Tracking the amount of energy you consume compared to your daily energy expenditure can help determine if your body is in an energy deficit. This is where the amount of energy consumed is less than the amount expended. Low energy availability reduces the ability of bone to resist load and/or impairs its ability to repair micro-damage [6]. Sustained periods of energy deficit can have negative effects on the body and will compromise performance and recovery. In females, this can lead to disorders in their menstruation cycle [6,7].
Assessing your attitude towards food can help to identify eating behaviours that may result in low energy availability. The Eating Attitudes Test (EAT-26) questionnaire is a simple screening tool that can help flag problematic eating behaviours [7]. Athletes that score 20 or higher on this test would benefit from professional guidance. The questionnaire can be found easily on google.
Risk factors: Vitamin D and calcium deficiency
Low vitamin D [1] and calcium levels were common findings in athletes that develop BSI [4,5,6]. Ensuring adequate levels via dietary intake or supplementation is an important factor, and a fairly easily achieved goal to help reduce BSI risk.
- 600 IU of vitamin D daily is suggested for ages 9 to 70 years
- 800 IU of vitamin D daily is recommended for > 71 years or older
- 1300 mg of calcium daily for ages between 9 to 18 years[11].
Conclusion
Bone Stress Injuries are painful injuries that are best avoided. It is important to be aware of the signs and symptoms of a BSI – particularly if you are new to running, have increased your training (especially after taking more than two weeks off running), and/or are at risk of any of the factors listed above. Developing a considered plan for your training load and recovery is crucial for avoiding this potentially season-ending injury. If you suspect you have a bone stress injury or have had one in the past, contact the intraining running injury clinic for an assessment and to develop a plan on how best to avoid them in future.
By Doug James – Physiotherapist and Podiatrist at intraining running injury clinic.

DOUG JAMES
PHYSIOTHERAPIST | PODIATRIST | L1 COACH
Doug James is a qualified physiotherapist and podiatrist with a special interest in running and sports injuries. He combines the two treatment approaches to achieve successful outcomes for clients of all abilities from non-athletes through to elite athletes.
Bachelor of Podiatry (Honours), Master of Physiotherapy Studies.
Doug has undertaken further training in dry needling, Pilates, and Rocktape and may incorporate these as necessary during treatment.
Doug is also a keen runner having completed the New York Marathon.
References:
- Alexandra Abbott, Mackenzie L. Bird, Emily Wild, Symone M. Brown, Greg Stewart & Mary K. Mulcahey (2020) Part I: epidemiology and risk factors for stress fractures in female athletes, The Physician and Sportsmedicine, 48:1, 17-24, DOI: 10.1080/00913847.2019.1632158
- Tavares, J., Jost, T., Drewelow, G., & Rylander, J. (2020). Do maximalist shoes mitigate risk factors for tibial stress fractures better than stability or flexible (marketed as minimalist) shoes? Footwear Science, 12(1), 63–74. https://doi.org/10.1080/19424280.2019.1708977
- Milner, C. E., Ferber, R. D., Pollard, C. S., Hamill, J., & Davis, I. (2006). Biomechanical Factors Associated with Tibial Stress Fracture in Female Runners. Medicine & Science in Sports & Exercise, 38(2), 323–328. https://doi.org/10.1249/01.mss.0000183477.75808.92
- Song SH, Koo JH. Bone Stress Injuries in Runners: a Review for Raising Interest in Stress Fractures in Korea. J Korean Med Sci. 2020 Mar;35(8):e38. https://doi.org/10.3346/jkms.2020.35.e38
- Miller, T. L., Kaeding, C. C., & Rodeo, S. A. (2020). Emerging Options for Biologic Enhancement of Stress Fracture Healing in Athletes. Journal of the American Academy of Orthopaedic Surgeons, 28(1), 1–9. https://doi.org/10.5435/JAAOS-D-19-00112
- Warden A, Davis I, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. J Orthop Sports Phys Ther. 2014;44(10):749e765. https://doi.org//10.2519/ jospt.2014.5334.
- Sanderson, S., Raab, S., & Moch, P. (2012). BMI and EAT-26, Predictors for Low BMD? SAGE Open, 2(1), 1–5. https://doi.org/10.1177/2158244012441604
- Gardner LI, Jr., Dziados JE, , Jones BH, , et al.. Prevention of lower extremity stress fractures: a controlled trial of a shock absorbent insole. Am J Public Health. 1988; 78: 1563– 1567.
- Snyder RA, , DeAngelis JP, , Koester MC, , Spindler KP, , Dunn WR. and Does shoe insole modification prevent stress fractures? A systematic review. HSS J. 2009; 5: 92– 98. http://dx.doi.org/10.1007/s11420-009-9114-y
- Salzler, M. J., Bluman, E. M., Noonan, S., Chiodo, C. P., & de Asla, R. J. (2012). Injuries Observed in Minimalist Runners. Foot & Ankle International, 33(4), 262–266. https://doi.org/10.3113/FAI.2012.0262
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. 1997.








 related to the way you run.
related to the way you run.










 Symptoms
Symptoms Diagnosis
Diagnosis

 How to use a foam roller?
How to use a foam roller?



 Clinically it has been suggested that LLCGs may also offer benefit in reducing muscle vibration that occurs during impact sports such as running, and this in turn could help reduce shin pain and calf muscle injuries.
Clinically it has been suggested that LLCGs may also offer benefit in reducing muscle vibration that occurs during impact sports such as running, and this in turn could help reduce shin pain and calf muscle injuries.

 Take the time to update your running shoes. Don’t leave it too late to change your shoes and risk getting an injury. As a general rule of thumb, the lifespan of a running shoe is
Take the time to update your running shoes. Don’t leave it too late to change your shoes and risk getting an injury. As a general rule of thumb, the lifespan of a running shoe is 


 4 Tips to manage and minimise the onset or severity of Sever’s Disease:
4 Tips to manage and minimise the onset or severity of Sever’s Disease:


 reputable running store and by knowledgeable staff who take the time to fit you up based on your needs. Trying the shoes on before you purchase them as well as receiving advice from trained experts will help you rest easy and know your next run will be an enjoyable one.
reputable running store and by knowledgeable staff who take the time to fit you up based on your needs. Trying the shoes on before you purchase them as well as receiving advice from trained experts will help you rest easy and know your next run will be an enjoyable one.

 Plantar Fasciitis is one of the most common complaints addressed by podiatrists among both runners and everyday individuals. Fasciitis refers to an acute presentation, whereas Fasciosis refers to more chronic pain. Pain is typically localised to the medial plantar heel (inside of the heel) at the insertion of the plantar fascia, and sometimes also extends through the medial (inside) arch of the foot. Although the plantar fascia is a soft tissue structure, it’s very inflexible and is responsible for containing the muscles of the foot, maintaining arch integrity and stabilising the foot during both stance and gait. The plantar fascia can quite easily become strained and overworked if your footwear is offering insufficient support, because the plantar fascia is working much harder to maintain it’s function.
Plantar Fasciitis is one of the most common complaints addressed by podiatrists among both runners and everyday individuals. Fasciitis refers to an acute presentation, whereas Fasciosis refers to more chronic pain. Pain is typically localised to the medial plantar heel (inside of the heel) at the insertion of the plantar fascia, and sometimes also extends through the medial (inside) arch of the foot. Although the plantar fascia is a soft tissue structure, it’s very inflexible and is responsible for containing the muscles of the foot, maintaining arch integrity and stabilising the foot during both stance and gait. The plantar fascia can quite easily become strained and overworked if your footwear is offering insufficient support, because the plantar fascia is working much harder to maintain it’s function. Posterior heel pain (Achilles injury)
Posterior heel pain (Achilles injury) Footwear again plays a significant role in resolving Achilles injuries. Structure and support are important, but targeting shoes with a higher heel pitch (difference in height/cushioning under the foot between the heel and forefoot) is most important. Increased heel pitch will reduce strain and stretch on the calves and Achilles, and promote active recovery during every day walking and standing without excessive load. Sometimes the opposite approach can be employed.
Footwear again plays a significant role in resolving Achilles injuries. Structure and support are important, but targeting shoes with a higher heel pitch (difference in height/cushioning under the foot between the heel and forefoot) is most important. Increased heel pitch will reduce strain and stretch on the calves and Achilles, and promote active recovery during every day walking and standing without excessive load. Sometimes the opposite approach can be employed. Plantar heel pain (underneath the central heel) can be caused by a number of injuries, with most being related to the calcaneal (heel) Fat Pad. The fat pad is designed to dampen impact forces and work as the body’s self-defence cushioning system. Fat Pad injury causes structural damage and jeopardises function, meaning that the heel bone is subjected to much larger impact forces in stance and during gait. Contusion (partial damage) or complete rupture may occur, with the later typically resulting from a sudden traumatic event such as landing very heavily (usually from a significant height) on a hard surface. Excessive load on the fat pad from long periods of standing or repetitive landings on an unforgiving surface can lead to contusion, particularly if footwear is not providing additional protection.
Plantar heel pain (underneath the central heel) can be caused by a number of injuries, with most being related to the calcaneal (heel) Fat Pad. The fat pad is designed to dampen impact forces and work as the body’s self-defence cushioning system. Fat Pad injury causes structural damage and jeopardises function, meaning that the heel bone is subjected to much larger impact forces in stance and during gait. Contusion (partial damage) or complete rupture may occur, with the later typically resulting from a sudden traumatic event such as landing very heavily (usually from a significant height) on a hard surface. Excessive load on the fat pad from long periods of standing or repetitive landings on an unforgiving surface can lead to contusion, particularly if footwear is not providing additional protection.


 Wearing the same pair of shoes day in and day out can cause significant and excessive wear, and inappropriate wear patterns to develop – especially when young, active children are the culprits. Children’s shoes are renowned for taking a beating in the schoolyard, and running shoes in particular are not designed to withstand the rigours of lunch-time play. Scuffing to the outsole and midsole can easily result from rough games and change of direction, whilst the lightweight, breathable upper is also easily damaged and does not provide sufficient support. Specific ‘school’ shoes will offer a more sturdy and hard-wearing outsole, and ideally a leather upper.
Wearing the same pair of shoes day in and day out can cause significant and excessive wear, and inappropriate wear patterns to develop – especially when young, active children are the culprits. Children’s shoes are renowned for taking a beating in the schoolyard, and running shoes in particular are not designed to withstand the rigours of lunch-time play. Scuffing to the outsole and midsole can easily result from rough games and change of direction, whilst the lightweight, breathable upper is also easily damaged and does not provide sufficient support. Specific ‘school’ shoes will offer a more sturdy and hard-wearing outsole, and ideally a leather upper.

 Each of these activities can hyper-extend the forefoot and can lead to plantar plate tear. Whilst not the sole cause, bio-mechanical issues are often a contributing factor to plantar plate tears, usually as a result of:
Each of these activities can hyper-extend the forefoot and can lead to plantar plate tear. Whilst not the sole cause, bio-mechanical issues are often a contributing factor to plantar plate tears, usually as a result of: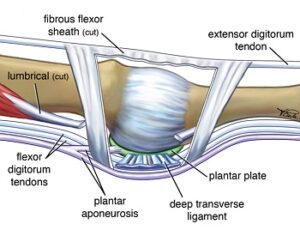 How to treat a plantar plate tear
How to treat a plantar plate tear